Who we are, why we’re on this journey, and why we’re sharing our story.
Mark and I met, fell in love, combined our families (my Chocolate Labrador and Aussie mix with his Corgi), and married because we decided we wanted to have a family. I met Mark while we were both volunteering in a program that helps veterans prepare for careers in high tech. We had both been in long-term relationships in the past that didn’t last. We knew rather quickly that we had something special and were honest about wanting to see where this relationship led.
I am older than Mark and knew my biological time to become a mother was drawing to a end. After many discussions and research, we decided to pursue reproductive assistance to have a child of our own. After a several IVF Cycles that failed, our successful IVF cycle ended on our honeymoon. We found out 10 days later that we were expecting! We had a healthy, but premature (due to me having severe preeclampsia in my 30th week of pregnancy) baby boy born at 33 weeks weighing 5lbs 2.5oz in January of 2018. He spent nearly a month in the NICU before we were able to take him home.
It’s an understatement to say we were relieved that our son and I survived the pregnancy. However, we were thrust into a confusing entry into parenthood in a frightening, beeping, sterile world of the NICU with our baby wearing an oxygen mask to help him breathe, fed by a feeding tube because he lacked the muscles to nurse or drink from a bottle, and seeing him connected to tubes and wires. NICU nurses and doctors, God bless their souls, taught us how to care for our small baby. It was stressful to make the hour long trek each way to the NICU everyday to hold my son in Kangaroo Care, attempt to pump breastmilk that barely dripped out into the tiny bottles, and support my baby in every way I could. However, I quickly realized my child was not only the giant of the NICU but he was well. Babies in Swedish Level IV are 6 to a NICU bay: I was surrounded by 1-2 lb preemies literally fighting for their tiny lives everyday. I remember crying and praying hour by hour – not for my own baby who just needed to grow and learn to suck, swallow, breathe – but for those miniature babies. I unintentionally overheard heard crisis events of their hearts stopping, resuscitation, hushed doctor-parent conversations, and the sobbing of parents. My heart broke for those babies and those parents. Those moments left an indelible mark on this momma’s heart. Mark and I looked at each other and decided never again. We couldn’t bear the idea of another complicated pregnancy where I might be at risk of losing my life, losing a baby, or watching a sick preemie struggle days, weeks, or months in the NICU. Never again, we said.
Long story told short, the experience of becoming parents to a preemie who eventually grew, despite preemie troubles (like frequent sickness because of an immune system that wasn’t as strong as his cohort and feeding troubles due to the neurology of preemies that predisposes them to sensory issues that lead to eating problems) into a curious, bright, and heart-melting toddler has been the most treasured and enriching experience of our lives. The first day he said, “I love you so much” to each of us, we couldn’t comprehend how much we could love this little boy more than we already did. Beyond being smitten with our toddler, we considered what his life would entail as an only child of two older parents with our nearest family thousands of miles away. How would his life change when we were gone? Who could he count on? Would he be alone?
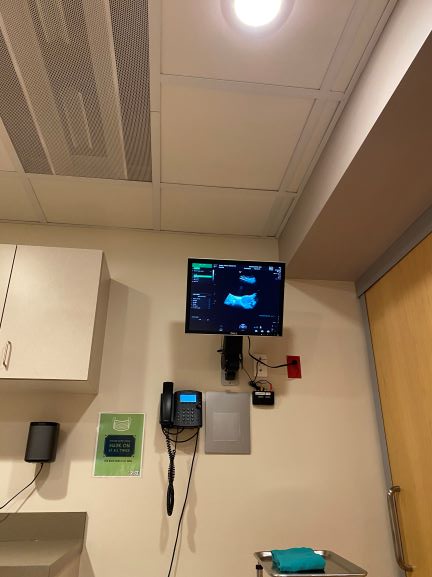
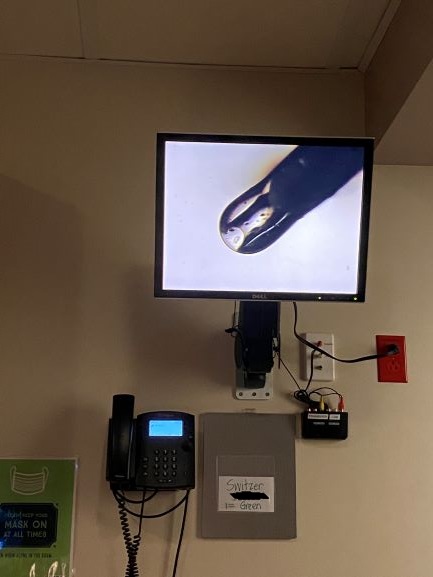
So, an idea began to take shape. We investigated with my SRM Reproductive team, my OBGYN, and discussed the risks of another pregnancy. Of all the complications that can go wrong, preeclampsia can be mitigated or delayed with close monitoring, preventive aspirin therapy, and possibly avoided. We had a plan and began our reproductive journey again in September of 2019. Little did we know what we would face.
As I’ve progressed in my pregnancy, the dream of an easy, happy, stress-free pregnancy evaporated. I began to find information and support for mono/di twin complications via the TTTS Foundation. At first, I didn’t understand why the women in the private groups would share such personal information or chose to blog about their experience. Yet As we’ve progressed farther into this world of mono/di complications, I now understand that we simply aren’t designed to shoulder such emotion and burden alone. Choosing to hide our journey away behind closed doors would not only be somehow acting as if we did something wrong, or brought these compilations upon ourselves, it would also deny the opportunity for prayer, love, and support from our family, friends, and most unexpectedly – strangers who have materialized along the way to show us unbelievable kindness. This is the story of our journey, written in real-time, as it continues to unfold told by me, Pamela, in an act of courage and attempt at catharsis and maintaining my sanity.