After months of discussions, calls, doctor’s appointments, medications and injections, the day has arrived for our Frozen Embryo Transfer (FET).
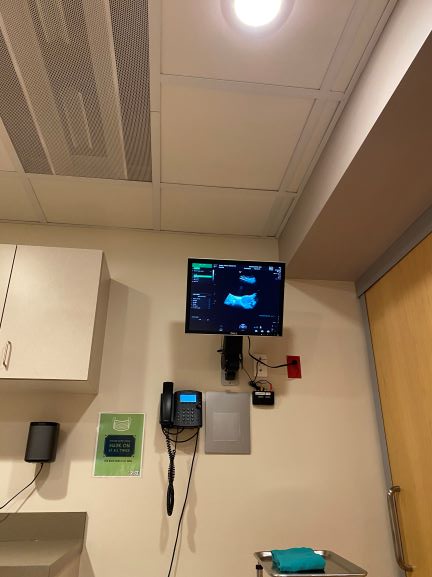
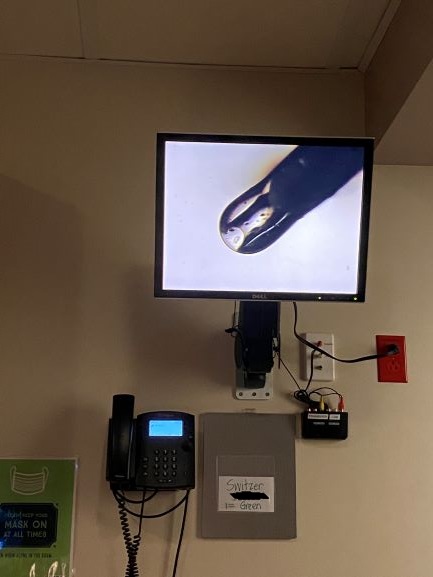
The day seemed like it was eagerly anticipated, yet it wasn’t quite what we’d pictured from our last embryo transfer. Having gone through this experience before, we had the ability to compare. In 2017, we’d arrived, parked, walked into the building, elevator, and clinic hand in hand. Our fertility doctor explained the procedure, the techniques, who would participate, and what to expect. Then it began and was complete in about 15 minutes of carefully orchestrated routine. The sliding door inner door in the exam room – the exam room that looked much like every other OBGYN exam room I’ve ever visited – opened directly into the embryology lab and an embryologist was waiting there standing in front of what appeared to be a clear isolation chamber that she could reach into. The monitor screen turned on and the image switched to a view looking down at the inside of the chamber and the embryologist’s hands. They showed a media dish shaped like a disk, with an identifying number on the disk (that number corresponded to my clinic identifier number and was checked and rechecked multiple times). As we watched on the monitor, she removed the lid, and zoomed in microscopically to a tiny image – technically the blastocyst – which was the embryo on Day 5 of its development after the egg was fertilized. While we watched, she drew the blastocyst into a clear tipped syringe and we followed its path easily out of the dish and into the tube. She then handed the syringe to our physician who had already readied the entry into my body with a common gynecological device. The monitor image switched to the ultrasound image, as a sonographer watched carefully. Our physician placed the syringe into my uterus, the sonographer measured the distance of the syringe tip to my uterine wall, called out the measurements and the physician depressed the plunger releasing the embryo in its saline bath into my uterus. She removed the syringe and speculum and that was the end of the procedure. I dressed, stopped by the ladies room on the way out, and Mark and I headed toward home.
This time, I had to make sure I had a surgical mask and my hand sanitizer in my purse before we left for the clinic because we were still enduring the COVID-19 pandemic, something we’d never anticipated at the start of all of our discussions. The traffic was extremely light on the way into downtown Seattle. Mark dropped me off at the front door, to park and wait outside because no one other than the patient was allowed inside the building. I waited alone for my name to be called. I went into likely the very same exam room, and the procedure was exactly the same as before with one exception. When the embryologist removed the lid to the media dish, she exclaimed “oh, it’s progressed since I peeked in this morning: it’s hatching and ready to implant!” I could swear as I stood up from the exam table to dress, I felt a lightning sharp pain in my uterus and felt the actual moment of implantation – which was surreal. I made my way out of the clinic and building and Mark picked me up at the curb. It was like much of our lives since COVID-19 arrived in our country, a new or adjusted reality. I may never use the word “normal” again.
We began the wait (also known as the 2 week wait) after IVF Embryo Transfer before our pregnancy test that would tell us if the procedure was successful.